Monkeypox virus is a viral infection caused by monkeypox virus (MPXV). This virus is spread primarily through contact with infected material and respiratory transmission. Monkeypox virus can cause infection in humans, which is a rare disease that is mainly endemic in Africa. Here is more information about monkeypox virus.
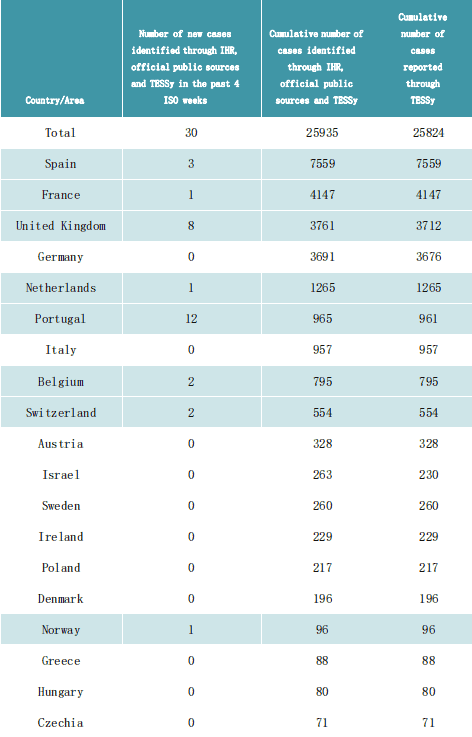
Monkeypox prevalence in various countries:
Joint ECDC-WHO Regional Office for Europe Mpox Surveillance Bulletin (europa.eu)
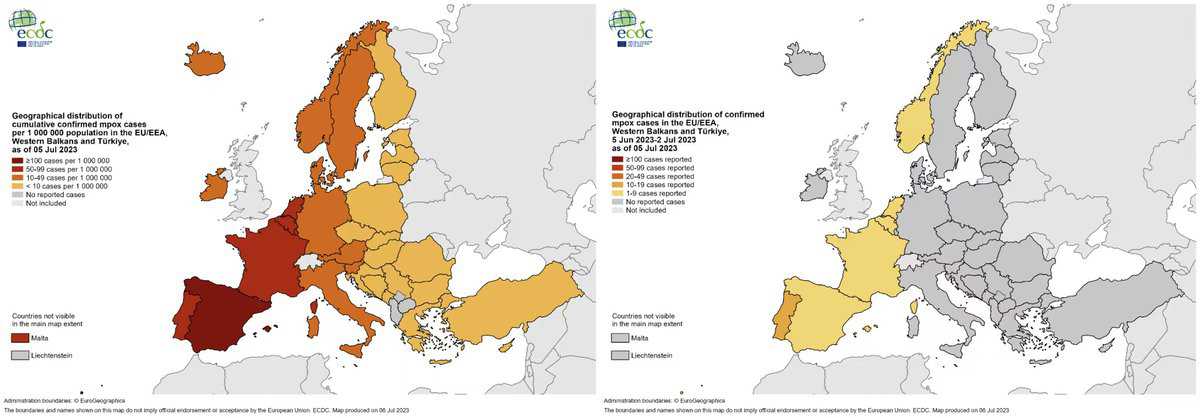
Surveillance summary
A total of 25,935 cases of mpox (formerly named monkeypox) have been identified through IHR mechanisms, official public sources and TESSy up to 06 July 2023, 14:00, from 45 countries and areas throughout the European Region. Over the past 4 weeks, 30 cases of mpox have been identified from 8 countries and areas.
Case-based data were reported for 25,824 cases from 41 countries and areas to ECDC and the WHO Regional Office for Europe through The European Surveillance System (TESSy), up to 06 July 2023, 10:00.
Of the 25,824 cases reported in TESSy, 25,646 were laboratory confirmed. Furthermore, where sequencing was available, 489 were confirmed to belong to Clade II, formerly known as the West African clade. The earliest known case has a specimen date of 07 March 2022 and was identified through retrospective testing of a residual sample. The earliest date of symptom onset was reported as 17 April 2022.
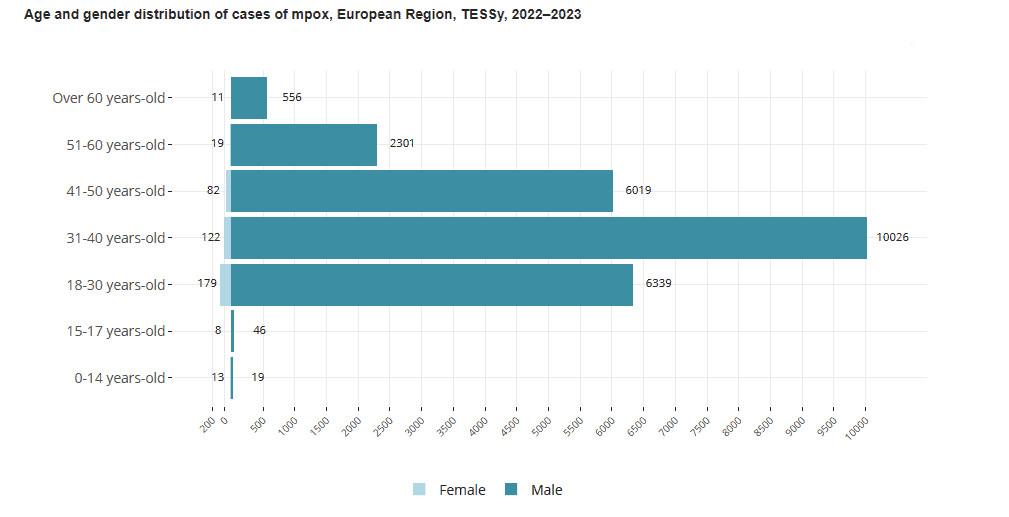
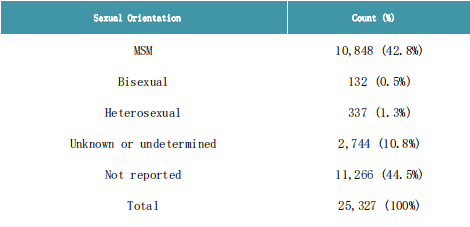
The majority of cases were between 31 and 40 years-old (10,167/25,794 – 39%) and male (25,327/25,761 – 98%). Of the 11,317 male cases with known sexual orientation, 96% self-identified as men who have sex with men. Among cases with known HIV status, 38% (4,064/10,675) were HIV-positive. The majority of cases presented with a rash (15,358/16,087 – 96%) and systemic symptoms such as fever, fatigue, muscle pain, chills, or headache (10,921/16,087 – 68%). There were 789 cases hospitalised (6%), of which 275 cases required clinical care. Eight cases were admitted to ICU, and seven cases of mpox were reported to have died.
To date, WHO and ECDC have been informed of five cases of occupational exposure. In four cases of occupational exposure, health workers were wearing recommended personal protective equipment but were exposed to body fluid while collecting samples. The fifth case was not wearing personal protective equipment. The WHO interim guidance on clinical management and infection prevention and control for mpox remains valid and is available at https://apps.who.int/iris/handle/10665/355798.
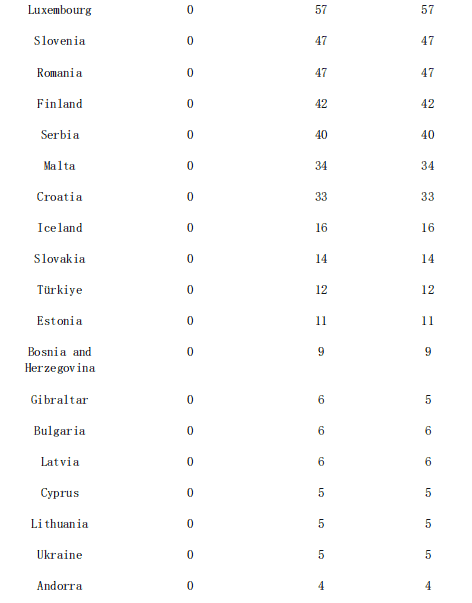
Summary of number of cases of mpox identified through IHR mechanisms and official public sources and reported to TESSy, European Region, 2022–2023
Countries and areas reporting new cases in the past 4 ISO weeks are highlighted in blue.
Summary of reported sexual orientations among male cases of mpox, European Region, TESSy, 2022–2023
Sexual orientation in TESSy is defined according to the following non-mutually exclusive categories:
- Heterosexual
- MSM = MSM/homo or bisexual male
- Women who have sex with women
- Bisexual
- Other
- Unknown or undetermined
Sexual orientation is not necessarily representative of the gender of the person the case had sex with in the past 21 days nor does it imply sexual contact and sexual transmission.
We summarize here the sexual orientation that male cases identified with.
Transmission
Person-to-person transmission of mpox can occur through direct contact with infectious skin or other lesions such as in the mouth or on genitals; this includes contact which is
- face-to-face (talking or breathing)
- skin-to-skin (touching or vaginal/anal sex)
- mouth-to-mouth (kissing)
- mouth-to-skin contact (oral sex or kissing the skin)
- respiratory droplets or short-range aerosols from prolonged close contact
The virus then enters the body through broken skin, mucosal surfaces (e g oral, pharyngeal, ocular, genital, anorectal), or via the respiratory tract. Mpox can spread to other members of the household and to sex partners. People with multiple sexual partners are at higher risk.
Animal to human transmission of mpox occurs from infected animals to humans from bites or scratches, or during activities such as hunting, skinning, trapping, cooking, playing with carcasses, or eating animals. The extent of viral circulation in animal populations is not entirely known and further studies are underway.
People can contract mpox from contaminated objects such as clothing or linens, through sharps injuries in health care, or in community setting such as tattoo parlours.
Signs and symptoms
Mpox causes signs and symptoms which usually begin within a week but can start 1–21 days after exposure. Symptoms typically last 2–4 weeks but may last longer in someone with a weakened immune system.
Common symptoms of mpox are:
- rash
- fever
- sore throat
- headache
- muscle aches
- back pain
- low energy
- swollen lymph nodes.
For some people, the first symptom of mpox is a rash, while others may have different symptoms first.
The rash begins as a flat sore which develops into a blister filled with liquid and may be itchy or painful. As the rash heals, the lesions dry up, crust over and fall off.
Some people may have one or a few skin lesions and others have hundreds or more. These can appear anywhere on the body such as the:
- palms of hands and soles of feet
- face, mouth and throat
- groin and genital areas
- anus.
Some people also have painful swelling of their rectum or pain and difficulty when peeing.
People with mpox are infectious and can pass the disease on to others until all sores have healed and a new layer of skin has formed.
Children, pregnant people and people with weak immune systems are at risk for complications from mpox.
Typically for mpox, fever, muscle aches and sore throat appear first. The mpox rash begins on the face and spreads over the body, extending to the palms of the hands and soles of the feet and evolves over 2-4 weeks in stages – macules, papules, vesicles, pustules. Lesions dip in the centre before crusting over. Scabs then fall off.Lymphadenopathy (swollen lymph nodes) is a classic feature of mpox. Some people can be infected without developing any symptoms.
In the context of the global outbreak of mpox which began in 2022 (caused mostly by Clade IIb virus), the illness begins differently in some people. In just over a half of cases, a rash may appear before or at the same time as other symptoms and does not always progress over the body. The first lesion can be in the groin, anus, or in or around the mouth.
People with mpox can become very sick. For example, the skin can become infected with bacteria leading to abscesses or serious skin damage. Other complications include pneumonia, corneal infection with loss of vision; pain or difficulty swallowing, vomiting and diarrhoea causing severe dehydration or malnutrition; sepsis (infection of the blood with a widespread inflammatory response in the body), inflammation of the brain (encephalitis), heart (myocarditis), rectum (proctitis), genital organs (balanitis) or urinary passages (urethritis), or death. Persons with immune suppression due to medication or medical conditions are at higher risk of serious illness and death due to mpox. People living with HIV that is not well-controlled or treated more often develop severe disease.
Infectious Disease
Monkey Pox Virus
Diagnosis
Identifying mpox can be difficult as other infections and conditions can look similar. It is important to distinguish mpox from chickenpox, measles, bacterial skin infections, scabies, herpes, syphilis, other sexually transmissible infections, and medication-associated allergies.
Someone with mpox may also have another sexually transmissible infection such as herpes. Alternatively, a child with suspected mpox may also have chickenpox. For these reasons, testing is key for people to get treatment as early as possible and prevent further spread.
Detection of viral DNA by polymerase chain reaction (PCR) is the preferred laboratory test for mpox. The best diagnostic specimens are taken directly from the rash – skin, fluid or crusts – collected by vigorous swabbing. In the absence of skin lesions, testing can be done on oropharyngeal, anal or rectal swabs. Testing blood is not recommended. Antibody detection methods may not be useful as they do not distinguish between different orthopoxviruses.
The Monkeypox Virus Antigen Rapid Test Kit is specifically designed for in vitro detection of the monkeypox virus antigen in human pharyngeal secretion samples and is intended for professional use only. This test kit utilizes the principle of colloidal gold immunochromatography, where the detection area of the nitrocellulose membrane (T line) is coated with mouse anti-monkeypox virus monoclonal antibody 2 (MPV-Ab2), and the quality control region (C-line) is coated with goat anti-mouse IgG polyclonal antibody and colloidal gold labelled mouse anti-monkeypox virus monoclonal antibody 1 (MPV-Ab1) on the gold-labelled pad.
During the test, when the sample is detected, the Monkeypox Virus Antigen (MPV-Ag) in the sample combines with colloidal gold (Au)-labelled mouse anti-monkeypox virus monoclonal antibody 1 to form an (Au-Mouse anti-monkeypox virus monoclonal antibody 1-[MPV-Ag]) immune complex, which flows forward in the nitrocellulose membrane. It then combines with coated mouse anti-monkeypox virus monoclonal antibody 2 to form agglutination “(Au MPV-Ab1-[MPV-Ag]-MPV-Ab2)” in the detection area (T-line) during the test.
The remaining colloidal gold-labelled Mouse anti-monkeypox virus monoclonal antibody 1 combines with goat anti-mouse IgG polyclonal antibody coated on the quality control line to form agglutination and develop colour. If the sample does not contain Monkeypox Virus antigen, the detection area cannot form an immune complex, and only the quality control area will form an immune complex and develop colour. This test kit includes detailed instructions to ensure that professionals can safely and effectively administer the test on patients within a 15-minute timeframe.